Please remember: the information presented on this website is intended for educational purposes and is not meant to replace a visit to a qualified healthcare provider.
Every day in my medical practice (usually multiple times), I see patients that request an antibiotic medication for the treatment of their symptoms. Most cases of infection seen by medical providers, do NOT require antibiotics for treatment. During a disaster situation, when medical care may not be readily available, it is important to use your preps wisely; therefore, in this post, we will review several basic indicators of infection, likely causes, and possible treatments.
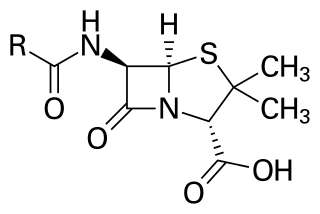
Penicillin core structure, where “R” is the variable group
Antibiotics kill bacteria (and some spirochetes), but not viruses. Except for some well known bacterial infections such as “strep throat”, “ear infections”, bacterial conjunctivitis (most people call this “pink eye”), urinary tract infections (UTI), tuberculosis (Tb), an infected cut, “food poisoning”, some STDs (chlamydia/gonorrhea) and certain types of pneumonia, many other common ailments are not bacterial. Most common infections experienced by adults and children are VIRAL.
There are several viral medications on the market that are focused on certain viral infections, examples include HIV, Hepatitis C, Influenza type A & B only (“the flu”), Herpes, and Shingles. Still, the treatments for these ailments don’t always “kill” the virus. Anti-viral medications generally control the quantity of virus present in the body by preventing the virus from multiplying, while the body’s immune system attacks the virus, or enhance the body’s immune system response in order to fight the virus.
As you may notice, a “cold” or “stomach bug” do not appear on the list of conditions that have viral medication available as treatment. Being told by a healthcare provider that you have a viral infection does NOT mean that you are not sick, it means an antibiotic will not work. In many cases, the main things that a healthcare provider can help you with are the treatment of your illness symptoms and instructing in ways to prevent complications, not in killing the virus. Therefore, the primary focus of a healthcare provider in treating viral illnesses will be symptom management and immune system support.
Just as a person prepares for major disasters or other potential life-disrupting events, 
These factors include:
- maintaining adequate hydration;
- having a healthy diet with an abundance of fruits and vegetables;
- getting adequate rest (studies show less than 6 hours of sleep per night increases the risk of chronic disease and decreases immune functioning);
- not smoking, taking illegal drugs, or drinking alcohol;
- having an adequate intake of vitamins and minerals necessary to promote the body’s peak performance;
- maintaining a healthy weight (not too thin, not too heavy);
- addressing and attentively managing any chronic medical conditions (Diabetes, COPD/asthma, seasonal allergies, colitis, HIV, etc.);
- avoiding persons with known or suspected contagious illness, whenever possible.

S. pyogenes bacteria at 900x magnification
Many bacterial infections are a secondary process. For example, a bacterial sinus infection will often follow a common cold or a time of seasonal allergy symptoms. Similar to a paper cut becoming infected, it happens with the passage of time, following the initial insult to the body. Studies demonstrate that for upper respiratory symptoms, generally the average time frame for developing a bacterial infection is 14 days. This is a general statistic and some patient-specific factors can contribute to a person’s risk of developing a bacterial infection more quickly (think diabetes, very old/very young,COPD/asthma, smoker, and other factors that effect the ability of the body’s immune system response).
As many people know, fever can be an indication of infection, but fever is not a specific symptom determining whether an infection is viral or bacterial. A fever is part of the body’s general defense system response. Sore throat, nasal congestion, diarrhea, cough and discolored mucous, are also not specific symptoms in determining a viral versus a bacterial cause of an illness. Remember during this discussion, not all scenarios can be addressed and there may be certain variables unique to your situation that are better evaluated by a healthcare provider.
So, you may be asking yourself: “How do I know whether or not I need antibiotics?”
Here are several questions that may help to determine this:
1. Was the initial onset of symptoms sudden? Or did the symptoms seem to improve, only to suddenly worsen?
2. Was there known illness exposure?
3. Have home remedies and over-the-counter (OTC) products helped improve comfort during the illness or do symptoms continue to worsen despite the use of these treatments?
4. Have symptoms been present for an extended period of time? (10-14 days for respiratory symptoms, >3 days for gastrointestinal (GI) symptoms or >5 days for skin symptoms).
 Generally, I advise my patients that the textbook sinus infection, for example, will follow a cold, flu or allergy “flare up”. Inadequate mucous clearance from the sinuses, following any of these occurrences, will set-up a person to have bacterial overgrowth and possibly a bacterial infection. Fever, fatigue, nasal congestion, colored OR clear nasal mucous, sore throat, post-nasal drip, facial pressure, headache, joint pain, general lymph node enlargement, and cough of sudden onset is the typical scenario of a common cold or influenza (“the flu”)–both viral illnesses. These symptoms generally will improve with the use of OTC preparations for cold/flu, as well as following general recommendations for rest, healthy diet, and hydration.
Generally, I advise my patients that the textbook sinus infection, for example, will follow a cold, flu or allergy “flare up”. Inadequate mucous clearance from the sinuses, following any of these occurrences, will set-up a person to have bacterial overgrowth and possibly a bacterial infection. Fever, fatigue, nasal congestion, colored OR clear nasal mucous, sore throat, post-nasal drip, facial pressure, headache, joint pain, general lymph node enlargement, and cough of sudden onset is the typical scenario of a common cold or influenza (“the flu”)–both viral illnesses. These symptoms generally will improve with the use of OTC preparations for cold/flu, as well as following general recommendations for rest, healthy diet, and hydration.
In contrast, a bacterial sinus infection may present as a sudden onset of symptoms following a cold in which a person may experience face pain/teeth pain, fatigue, bloody nasal discharge, sore throat, foul-smelling breath, changes in taste/smell, and headache (especially focused in a sinus location), and which are unrelieved with OTC pain relievers or decongestants. An antibiotic may be indicated in this situation, if the actions to clean out the excess mucous from the sinuses have not been successful or if they have not improved the severity of the symptoms.
During a viral illness or allergy flare, the primary treatment goals are to promote comfort, thin  mucous in order to prevent a collection that would harbor bacterial growth, improve the clearance of mucous from the body, and provide the necessary conditions for the immune system to function. Taking OTC pain and fever relievers (for example acetaminophen, ibuprofen, naproxen, etc) may help with the joint pain, fever, headache. Peppermint oil applied to the skin via a carrier oil, can also help with fever and headache. Increasing intake of healthy fluids (those that are non-alcoholic and non-caffeinated), using humidified air, nasal saline spray, sinus rinses, nasal steroid sprays (fluticasone, betamethasone), and guaifenesin, are examples of methods that may help to thin mucous and eliminate it from the sinuses. Essential oils including menthol, peppermint, eucalyptus, melaleuca, and rosemary can help improve respiratory comfort, whether diffused into the air or applied topically to the skin via a carrier oil. Salt water gargles, throat lozenges, numbing throat sprays, and cold liquids can all help to improve the discomfort of a sore throat from whatever cause. Cough drops and warm liquids can help ease the discomfort from a cough. If the cough is interfering with adequate rest, then a cough suppressant can be helpful (ie., dextromethorphan).
mucous in order to prevent a collection that would harbor bacterial growth, improve the clearance of mucous from the body, and provide the necessary conditions for the immune system to function. Taking OTC pain and fever relievers (for example acetaminophen, ibuprofen, naproxen, etc) may help with the joint pain, fever, headache. Peppermint oil applied to the skin via a carrier oil, can also help with fever and headache. Increasing intake of healthy fluids (those that are non-alcoholic and non-caffeinated), using humidified air, nasal saline spray, sinus rinses, nasal steroid sprays (fluticasone, betamethasone), and guaifenesin, are examples of methods that may help to thin mucous and eliminate it from the sinuses. Essential oils including menthol, peppermint, eucalyptus, melaleuca, and rosemary can help improve respiratory comfort, whether diffused into the air or applied topically to the skin via a carrier oil. Salt water gargles, throat lozenges, numbing throat sprays, and cold liquids can all help to improve the discomfort of a sore throat from whatever cause. Cough drops and warm liquids can help ease the discomfort from a cough. If the cough is interfering with adequate rest, then a cough suppressant can be helpful (ie., dextromethorphan).
A bacterial sinus infection would continue to benefit from these interventions in addition to any antibiotic therapy. A good analogy for treating a bacterial sinus infection would be: When you have standing water in the back yard in the summer time, mosquitoes will flourish there. Pouring bleach into the standing water will kill the mosquitoes, but if the standing water is not eliminated, the mosquitoes will return.
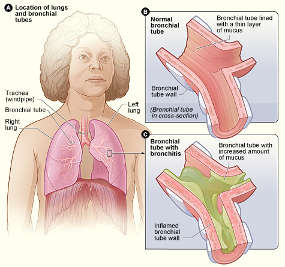
Similar reasoning can be applied to lower respiratory illnesses like bronchitis. Generally,
acute bronchitis, in an otherwise healthy person, is most often a viral infection; hence antibiotics would be ineffective as a treatment. However, failure to adequately clear mucous from the airways or to mount a strong immune response, could lead to a bacterial infection developing. Again, because it takes time for bacterial overgrowth to occur, studies do not generally support the need for antibiotics as treatment for bronchitis until symptoms have been present for 10 to 14 days. As stated previously, there are exceptions to this when considering persons with chronic diseases that impact the lungs or those with an impaired immune response. The interventions listed above for upper respiratory infection would also be helpful in treating lower respiratory illnesses. In addition, bronchodilator medications (for example, albuterol and levalbuterol) can be helpful to open the airways and allow mucous to be more easily expelled from the body, thereby decreasing mucous retention, bacterial overgrowth and a bacterial infection.
Please note: Decongestant nasal sprays (ie, oxymetazoline–brand named Afrin) are not to be used beyond 3 days, as they can contribute to the development of other problems. Oral decongestants (ie, pseudoephedrine–brand named Sudafed) and bronchodilator medications may not be safe for use in people with high blood pressure or other cardiovascular disease.
In conclusion, there is not a one-size-fits-all solution for illnesses. Knowing which illnesses may require antibiotics and which may not, is an important distinction in planning and utilizing your preps. There is no magic pill in medicine. We do not have all the answers and there is no Star Trek-like scanner that can diagnose and treat medical conditions. Using a logic-based methodical approach to diagnosis and treatment is the best.
A broad “rule-of-thumb” when treating most illness is: Think horses, not zebras.
Think common, before uncommon. (Of course, if you live in a part of the world where the reverse is true, then this axiom wouldn’t apply, but for much of the world it does).
In future posts, a variety of medical topics will be covered regarding the treatment of common illnesses and other health-related situations, with the hope that sharing basic health-related information will improve the readiness of people in times when medical care may not be accessible.
External Resources:
http://www.webmd.com/cold-and-flu/video/josephson-antibiotics
http://www.webmd.com/cold-and-flu/cold-guide/antibiotics-colds
https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm092810.htm
http://www.aafp.org/afp/2001/0915/p999.html